With the aging of the U.S. population, nontuberculous mycobacterial lung disease and bronchiectasis are on the rise, with diagnoses for both conditions growing by approximately 8 percent a year, according to recent studies. This has prompted Johns Hopkins pulmonologists Keira Cohen and Mark Jennings to launch a multidisciplinary center to manage and study these conditions.

“A lot of these patients have seen multiple specialists and have had a difficult time finding a place where they can get adequate care,” Jennings says, in part because of challenges in making the correct diagnosis. In many cases the symptoms can be nonspecific, like a chronic cough. “We think it’s important to provide not only care but also an infrastructure in which meaningful research can be done to advance treatments.”

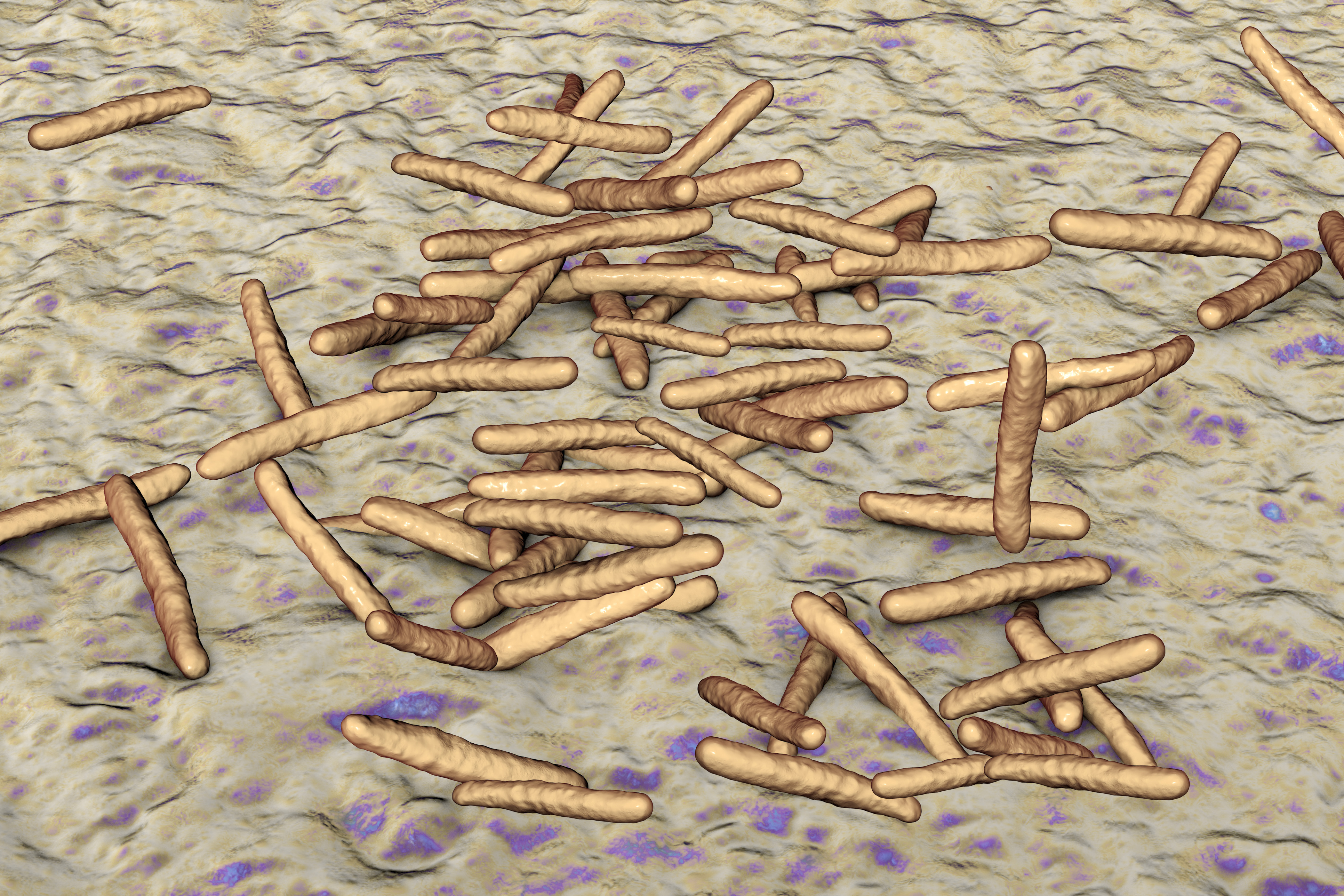
Although nontuberculous mycobacteria, or NTM, occur naturally in the environment and do not cause health problems for most people, certain individuals are unusually vulnerable to these organisms, which can infect the airways and lung tissue. Those who require NTM treatment may be prescribed a regimen of multiple antibiotics for over a year. NTM is now the dominant mycobacterial disease in the U.S., says Cohen, although the infections are not generally thought to pass from person to person like tuberculosis: “We hear a lot about TB, but we have approximately 10 times as many cases of NTM disease than TB these days.”
Share Fast Facts
“For patients traveling to Johns Hopkins, the convenience of having us all in one place can’t be underestimated,” says pulmonologist Keira Cohen. Click to Tweet
Bronchiectasis can develop from multiple causes and, if not managed well, can lead to worsening lung function due to airway scarring and chronic infection. “These patients are at risk for all sorts of infections but one that we see in particular is NTM,” says Jennings, so it made sense for their new center to focus on both conditions. “Patients are incredibly sick and have a lot of highly specialized clinical needs. They warrant a real clinical home.”
At the Johns Hopkins Center for Nontuberculous Mycobacteria and Bronchiectasis, which operates Friday mornings at Johns Hopkins Bayview Medical Center, patients can see Jennings, Cohen, Jonathan Zenilman (an infectious diseases specialist skilled at managing mycobacterial infections) and physical therapists knowledgeable about airway clearance techniques. “For patients traveling to Johns Hopkins, the convenience of having us all in one place can’t be underestimated,” Cohen says.
Due to the complexities involved in managing these conditions, and because a range of diseases can lead to bronchiectasis, the center also works with a chest radiologist and has relationships with specialists in rheumatology, allergy and immunology, gastroenterology and otolaryngology. The Johns Hopkins Clinical Mycobacteriology Lab allows Cohen and Jennings to accurately assess test results.
Cohen and Jennings also made a commitment to research. Currently, clinical outcomes for both NTM and bronchiectasis nationwide are poor, Cohen says. “We can and should be doing better, but in order for us to do better, we need to learn more about these interrelated diseases.”
Every patient coming to the Johns Hopkins center is offered the opportunity to participate in clinical research. The center has an ongoing prospective study and biobank collecting blood, sputum and other samples from patients. Cohen has two studies investigating drug resistance mechanisms in NTM and one investigating blood-based biomarkers of Mycobacterium avium lung disease.
The center also is entering clinical trials for new and existing therapies. Jennings is the local principal investigator for a multicenter phase II trial of a novel therapy for non-cystic fibrosis bronchiectasis. He and Cohen are in talks to take part in future trials of novel therapies for NTM.
“Ultimately, our goal is to advance care and improve outcomes, not just of the patients we are going to see in clinic but more broadly,” Jennings says.
