Virulent E .coli outbreaks aren’t anything to fool with, says molecular biologist Olga Kovbasnjuk. In 2011, for example, a European outbreak brought 51 deaths from hemorrhagic colitis or kidney failure. It touched nearly 4,000 people in 16 countries. “Bacteria thatcarry the Shiga toxin are major foodborne pathogenswith no effective therapy,” Kovbasnjuk explains.
And so Kovbasnjuk has made inroads in clarifying the early pathology of enterohemorrhagic E. coli, when the infection is likely best tackled. A new patent for a therapeutic approach is now on the way.
Specifically, she’s tackled the major question, how does the toxin put out by this dangerous E. coli cross the gut wall and get into the bloodstream? It’s known that bacteria release Shiga toxin and the molecule subsequently gets taken in by the gut’s enterocytes. Shiga toxins traverse the cells, then slip into the bloodstream. Once there, they prompt an immune response and inflammation.
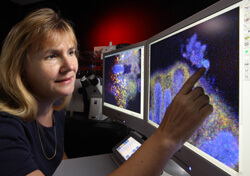
What starts this? Something about the bacterial presence trips a structural shift in the host cell membrane, says Kovbasnjuk. Her confocal imaging shows outpocketing of the apical membrane followed by large, toxin-carrying vacuoles appearing inside the cells (see back page). The lab’s most recent study, soon to be published, suggests that a soluble bacterial enzyme, serine protease, alters gut cells to trigger their enfolding of the toxin.
Most satisfying to Kovbasnjuk is “our ability to block serine protease.” A patent is on the way, she says, of an agent able to halt Shiga toxin uptake, “and, we hope, a way to prevent this disease.”
Kovbasnjuk also speaks of a new technique that’s “really quite amazing.”
Three years ago Dutch researchers plucked interstitial stem cells from the crypts they biopsied from human small bowel. They showed that the cells could evolve into clumps, then into roughly crypt-shaped enteroids. The tiny, free-floating sacs carry hallmarks of adult human crypts. “And they’re justwhat we’ve been needing to study intestinal disease, to test drugs and before long, to develop tailored therapies for patients,” says Kovbasnjuk.
Under an NIH grant, her lab developed a reliable technique for growing enteroids and “proving” them. Their electron micrographs verify cells’ apical membranes with brush borders, basal membranes and the proper cuboidal shape. “Human enteroids advanced our knowledge,” Kovbasnjuk says. “Now they let us test potential therapy.”
