BUFFALO, N.Y. and FAIRFAX, Va. — The vast majority of ovarian cancers, about 70%, don’t become apparent until they are advanced, making the chance of successful treatment to control these tumors quite slim. Four top teams of ovarian cancer researchers are uniting efforts in an unprecedented collaboration aimed at enabling early detection and perhaps prevention of many ovarian cancers. Funded by a developmental grant from the U.S. Department of Defense (DoD), the initiative will bring together researchers from both government and academic centers to apply emerging technologies to this pressing challenge to discover biomarkers for early detection of ovarian cancer.
The initiative, known as the DoD and SPORE Ovarian Cancer Omics Consortium, or DSOCOC, hinges on recent discoveries about the origins of ovarian cancers and on omics, an umbrella term for new sequencing-based approaches that enable the deep characterization of various types of molecules that play important roles in human biology.
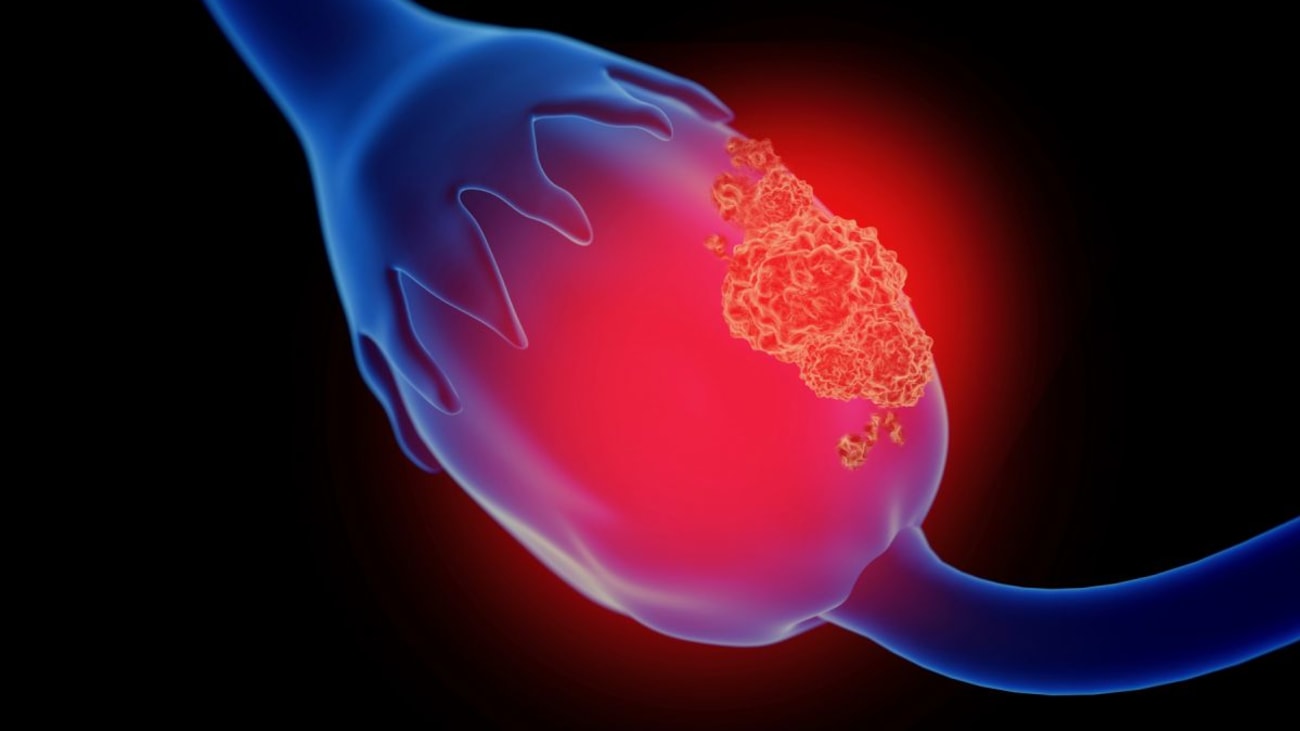
“Recent research has implicated the fallopian tubes as the source of many ovarian cancers. Cells toward the end of the fallopian tube take on malignant features, then drop these mutated cells on the surface of the ovary and within the abdominal cavity, where they have the opportunity to develop into aggressive and hard-to-detect cancers,” says Kunle Odunsi, MD, PhD, FRCOG, FACOG, Deputy Director of Roswell Park Comprehensive Cancer Center, who will lead the collaborative effort as principal investigator (PI).
These lesions, known as serous tubal intraepithelial carcinoma, or STIC — the precursors of the majority of ovarian cancers — take about seven years to develop, but are rarely found at early stages, before they evolve into cancer.
“We’re asking the question, ‘Can we identify STIC lesions long before they become cancer as a form of early detection, similar to a PAP smear?’ There’s a window of opportunity where, if we can identify STICs, we can potentially prevent ovarian cancer, and that’s the challenge these accomplished teams are coming together to tackle using state-of-the-art omics technologies,” says Dr. Odunsi, who is also Chair of the Department of Gynecologic Oncology, the M. Steven Piver Professor of Gynecologic Oncology and Executive Director of the Center for Immunotherapy at Roswell Park, which is based in Buffalo, N.Y.
Larry Maxwell, MD, Chair of Obstetrics and Gynecology at Inova Fairfax Women’s Hospital, is co-PI of the new effort as well as co-PI for the Department of Defense (DoD) Gynecologic Cancer Center of Excellence (GYN-COE).
“I don’t believe there has ever been such a united effort in medical science among researchers from both government and academic research organizations,” notes Dr. Maxwell, a retired Army Colonel who is also a Professor at the Uniformed Services University of the Health Sciences as well as the University of Virginia. “This project will rely on expertise and resources that could only be realized through such a cooperative and collaborative effort. We’re able to set our sights much higher by working together and creating a force multiplying synergy.”
This initial phase of work, funded by a $544,360 grant from the DoD (award number W81XWH-19-1-0183), will focus on setting up the infrastructure and teams to enable this ambitious effort. Longer-term goals focus on gathering and harmonizing biospecimens and discovering and validating biomarkers to inform early detection and screening for STIC and ovarian cancer.
The Consortium will be comprised of the GYN-COE and Women’s Health Integrated Research Center at Inova along with the three teams nationally that are pursuing federally funded research in ovarian cancer as part of the National Cancer Institute’s Specialized Programs of Research Excellence (SPORE) initiative:
- Roswell Park Comprehensive Cancer Center in collaboration with the University of Pittsburgh Cancer Institute, led by Dr. Odunsi, overall PI, and Kirsten Moysich, PhD, co-PI and epidemiologist/public health expert
- The Mayo Clinic Cancer Center, led by Scott Kaufmann, MD, PhD, PI, and Mark Sherman, MD, Biospecimen Core Leader
- MD Anderson Cancer Center, led by co-PIs Robert Bast, MD, and Anil Sood, MD
The Consortium will also be guided by the input of a six-member Patient Advisory Council chaired by Mary Jackson Scroggins, MA, and will work closely with the Society of Gynecologic Oncology and patient advocacy groups around the country.
“This will be a multi-year effort that will rely on the contributions and participation of hundreds of people around the country,” notes Dr. Odunsi. “Our hope is that through team science, state-of-the-art technology and grassroots advocacy we will be able to dampen the impact of this very deadly and devastating cancer.”
Roswell Park Comprehensive Cancer Center is a community united by the drive to eliminate cancer’s grip on humanity by unlocking its secrets through personalized approaches and unleashing the healing power of hope. Founded by Dr. Roswell Park in 1898, it is the only National Cancer Institute-designated comprehensive cancer center in Upstate New York. Learn more at www.roswellpark.org, or contact us at 1-800-ROSWELL (1-800-767-9355) or ASKRoswell@RoswellPark.org.
