Johns Hopkins among few centers in U.S. to offer spectrum of lymphatic reconstruction and ablation procedures for patients who fail initial treatments.
Although surgery for lymphedema is common, institutions that offer the entire suite of surgical options at a single location — as Johns Hopkins does — are rare, says Oluseyi Aliu, a Johns Hopkins plastic and reconstructive surgeon. Aliu specializes in treatment of advanced lymphedema, offering relief to patients who have few avenues left.
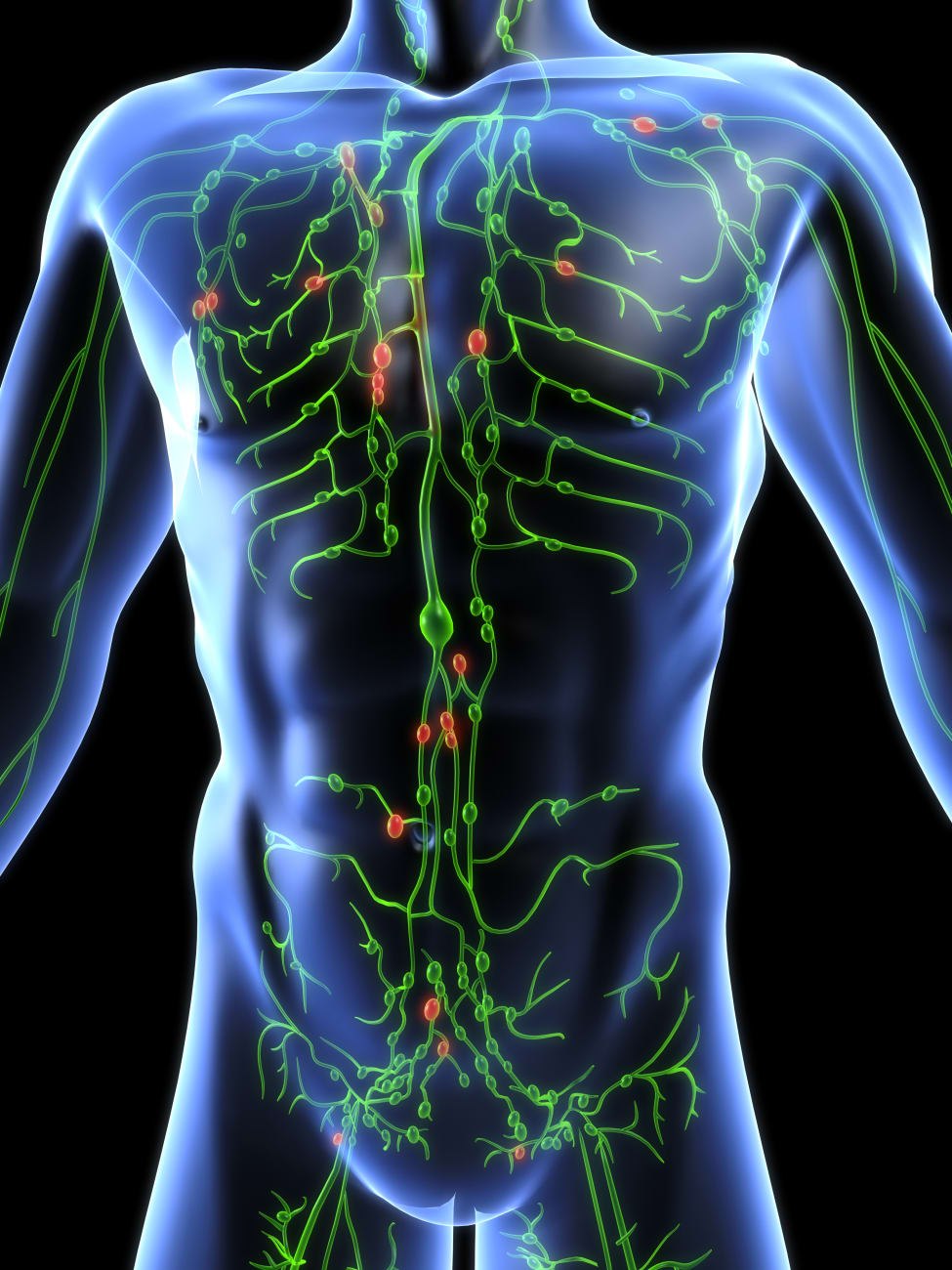
For most patients, the condition results from secondary causes — trauma, or cancer treatments that remove or damage lymph nodes in the axilla or groin. A minority of patients have primary lymphedema, a congenital or developmental condition that often arises during adolescence or early adulthood.
Typically, initial treatments attempt to mechanically push fluids out of the affected limb with compression devices or garments, or use physical therapy that encourages drainage. But over time, explains Aliu, many patients stop responding to these treatments. As fluid builds up in the affected limb, it causes a vicious cycle of inflammation, fibrosis and further damage to lymphatic vessels, making them even more inefficient at returning lymphatic fluid to the circulation.
“When patients reach the point when the disease stops responding to nonsurgical treatments,” Aliu says, “that’s when they come see us.”
Surgical treatments fall into two broad categories: those for patients with some degree of lymphatic function and those without. Aliu deciphers the two with an indocyanine green (ICG) lymphography, a test he performs in-office during which dye that can be detected with an infrared camera is injected into the local lymphatic system. Through this diagnostic procedure, Aliu offers same-day assessment that helps guide treatment — a boon for patients who travel to Johns Hopkins from out of state or another country.
For patients with still functioning lymphatic channels in the affected limb, Aliu and colleagues — a group of five microsurgeons specializing in lymphedema reconstruction — can reroute these channels to connect with adjacent veins, bypassing unhealthy lymphatic vessels. For those without any functioning channels in the limb, the surgeons may be able to harvest healthy lymph nodes from elsewhere in the body and transplant them to reinvigorate lymphatic function.
Patients with advanced disease who aren’t eligible for these procedures are often candidates for debulking or ablative surgery, Aliu says. These operations reduce the limb’s size by removing damaged tissue, often shrinking it by a third or more. Making the limb smaller helps the patient attend to daily life much more comfortably.
Aliu adds that he and his colleagues are working to improve the care they deliver through studies tracking patient-reported outcomes. Learning more about patients’ experiences and treatment goals informs their care discussions with new patients.
When patients initially see him, Aliu says, they’re often dejected from years of suffering. After treatment, many have such relief that Aliu can almost feel it himself.
“I can’t offer them a cure, but I can give them something that can significantly change their lives,” Aliu says.
Visit the lymphedema surgery website.
To refer a patient, call 443-997-9466.